Data Owners vs Stewards vs Custodians: Roles Explained
Post Summary
When managing healthcare data, three key roles ensure everything runs smoothly: Data Owners, Data Stewards, and Data Custodians. Each has distinct responsibilities:
- Data Owners: Senior leaders responsible for setting policies, ensuring compliance (e.g., HIPAA), and aligning data with organizational goals.
- Data Stewards: Focus on maintaining data accuracy, consistency, and quality. They enforce policies and handle day-to-day data management tasks.
- Data Custodians: Technical experts who manage systems, enforce security measures (e.g., encryption), and ensure data is stored and protected properly.
These roles work together to safeguard sensitive healthcare information, prevent data breaches and ransomware, and ensure compliance with regulations. Below, we’ll break down their responsibilities, skills, and how they collaborate to manage healthcare data effectively.
What Is Data Governance? Framework, Roles, Pillars and Best Practices
sbb-itb-535baee
Data Owners: Decision-Making and Accountability
Data owners are at the pinnacle of the healthcare data governance structure. These senior executives, such as department heads, carry the ultimate responsibility for how specific datasets are classified, safeguarded, and utilized [4][5]. Unlike technical teams, their focus is on shaping the strategic framework that guides data management across the organization.
Ben Herzberg, Chief Scientist at Satori, captures the essence of their role:
"While data can be a resource shared by several stakeholders, accountability for Data Governance is never shared: it is solely the Data Owner's responsibility." [5]
This responsibility goes beyond mere oversight. In healthcare, where a single cancer patient's genetic data can reach approximately one petabyte - over a billion megabytes - data owners must juggle regulatory compliance with forward-thinking strategies. They act as a vital link between senior leadership and the data governance council, ensuring that the organization’s data policies align with broader institutional goals [6]. Their work sets the stage for collaboration with stewards and custodians. Let’s dive into their main responsibilities and the skills they bring to the table.
What Data Owners Do
Data owners drive the strategic vision for data governance, setting the direction while delegating the operational details to data stewards [5][6]. Their responsibilities include creating and enforcing policies that ensure compliance with regulations like HIPAA and GDPR [4]. They define role-based access controls, establish data retention guidelines, and outline protocols for addressing data-related issues.
They also oversee systems to monitor, audit, and report on data quality [4][5]. When problems arise, data owners allocate the necessary resources and budget for corrective measures, such as audits or data cleansing initiatives [4][5]. Additionally, they ensure that all stakeholders agree on a standardized data glossary, adhering to frameworks like ISO 15489 [5][7].
Required Skills and Knowledge
To effectively carry out their role, data owners must hold senior authority [4][5][6]. This position requires someone in upper management who can enforce changes across departments and secure funding for data initiatives [5][6].
A deep understanding of healthcare regulations is essential. They need to be well-versed in HIPAA, GDPR, and how these laws apply to their organization’s datasets [3][6]. Strong leadership skills are critical, enabling them to coordinate efforts among business stakeholders, IT teams, and clinical staff. Strategic planning is another key component, allowing them to balance organizational goals with regulatory compliance. DataSunrise describes their role succinctly:
"The data owner is the cornerstone of data governance - ensuring that information assets are aligned with business goals, well-governed, and available for decision-making when it matters most." [4]
Data Stewards: Quality and Accuracy Management
In the healthcare data governance framework, stewards play a vital role in executing the policies established by data owners to uphold data quality. Data stewards are the operational backbone of data governance. While owners focus on setting the strategic direction, stewards handle the day-to-day tasks like quality checks, metadata management, and ensuring the integrity of the data [8][9].
"Data stewardship can be considered 'the operational aspect' of data governance." [8]
This role has grown in importance as the healthcare industry now generates nearly one-third of the world’s data [10]. Stewards ensure that this massive amount of information remains reliable - whether it’s being used for diagnosing patients, meeting regulatory requirements, or training AI systems that depend on clean, unbiased datasets [8][1]. Below, we explore the specific responsibilities that stewards take on to maintain these high standards.
What Data Stewards Do
Data stewards focus on ensuring accuracy and consistency in healthcare data. They perform data profiling to spot anomalies, create validation rules (like confirming lab results fall within acceptable ranges), and clean up duplicate or incomplete records [8][1]. For example, they resolve inconsistencies like differing marital status codes to maintain uniformity [8].
Another critical area they manage is metadata, which helps maintain audit trails and allows clinical staff to verify the reliability of patient information [8][9][1].
Real-world examples illustrate the impact of their work. In 2024, a SaaS company introduced dedicated stewards for its core data domains. Within six months, they achieved a 45% reduction in duplicate records, cut the time to merge data from 10 days to just 48 hours, and improved sales forecast accuracy by 9 percentage points [9].
Stewards also handle compliance with regulations like HIPAA, manage consent records, and ensure data retention aligns with GDPR and the 21st Century Cures Act [10][1]. Additionally, they work on interoperability by setting common data standards that enable secure information exchange between hospitals, labs, and insurance providers [10][1].
Working with Owners and Custodians
Beyond their operational duties, stewards serve as the bridge between strategic goals and technical execution. They translate the policies set by data owners into actionable standards, quality metrics, and access controls for data custodians to implement [9][4]. As The Pedowitz Group explains:
"The owner is accountable for policy and outcomes; the steward operationalizes standards, quality, metadata, access, and retention." [9]
To clarify roles, stewards often use tools like RACI matrices. In this framework, owners are "Accountable" for policy decisions, stewards are "Responsible" for maintaining data quality and standards, and custodians are either "Consulted" or "Informed" about technical implementations [9].
Stewards also identify authoritative systems, such as designating an electronic health record as the official source for patient demographics. This helps custodians configure infrastructure accordingly [9].
Dashboards with SLAs are another tool stewards use to set clear remediation targets. By maintaining transparent data lineage, they enable technical teams to track data transformations and resolve issues efficiently [9][1]. This collaborative approach ensures governance policies are not just theoretical but actively applied in healthcare systems.
Data Custodians: Technical Systems and Security
While data stewards focus on ensuring data quality and adherence to standards, data custodians handle the technical side of things. Their primary responsibility is to manage the systems that store and protect healthcare information. This includes turning high-level policies into actionable systems - like managing databases, implementing encryption, and restricting access to electronic protected health information (ePHI) to authorized users only. Shelley Bougnague from Cloudficient captures this role perfectly:
"A data custodian is the steward of an organization's data environment, translating high-level policies into practical systems and controls." [12]
Data custodians often have roles like Database Administrator, Data Engineer, or System Administrator. Their work is essential. For instance, a resolution agreement was reached by the Office for Civil Rights with a covered entity after it was found that ePHI for over 3,000 individuals had been stored on a cloud server without a required Business Associate Agreement [13].
What Data Custodians Do
Data custodians are the go-to experts for the technical operations that ensure healthcare data remains both secure and accessible. One of their key tasks is managing access controls. This includes assigning unique user IDs, enforcing multi-factor authentication, and setting automatic logoffs after 90 minutes of inactivity, as per CMS policy. For high-risk users in "High" level systems, access must be disabled within 30 minutes of detection, and accounts for terminated employees are removed within 30 days [11].
Another critical area is data protection. Custodians implement encryption for both data at rest and data in transit. Tools like AWS Key Management Service (KMS) and TLS 1.2+ are commonly used to secure data transfers. They also ensure accurate backup copies of ePHI are created and maintain disaster recovery protocols to restore data during system failures.
Monitoring and audit controls are equally important. Custodians use Security Information and Event Management (SIEM) tools to track and analyze system activity involving ePHI. These tools help identify unusual behaviors, such as unexpected data transfers or access during odd hours. Integrity controls are also deployed to confirm that ePHI remains unaltered. This combination of responsibilities requires a deep understanding of technical systems.
Technical Skills and Tools Needed
To meet these demands, data custodians need a robust technical skill set. Their expertise must align with HIPAA's five safeguards: access controls, audit controls, integrity measures, authentication, and transmission security. Proficiency with Identity and Access Management systems - like Active Directory, OAuth2, and multi-factor authentication tools such as PIV cards or RSA tokens - is essential.
Knowledge of network architecture is another must. Custodians often configure Virtual Local Area Networks (VLANs) to separate security zones and manage encrypted message queues. They also need to understand compliance frameworks like NIST SP 800-53, HIPAA, and FISMA to translate regulatory requirements into effective technical configurations.
Practical tools and methods play a big role in their daily work. For instance, Infrastructure as Code (IaC) helps enforce encryption when creating new environments, while automated remediation tools detect and fix unsecured resources. Service Control Policies are used to maintain data locality. In healthcare organizations that rely on a complex web of vendors, platforms like Censinet RiskOps™ enable custodians to manage technical risk assessments and ensure third-party systems handling PHI follow consistent security controls across the board.
Comparing Data Owners, Stewards, and Custodians
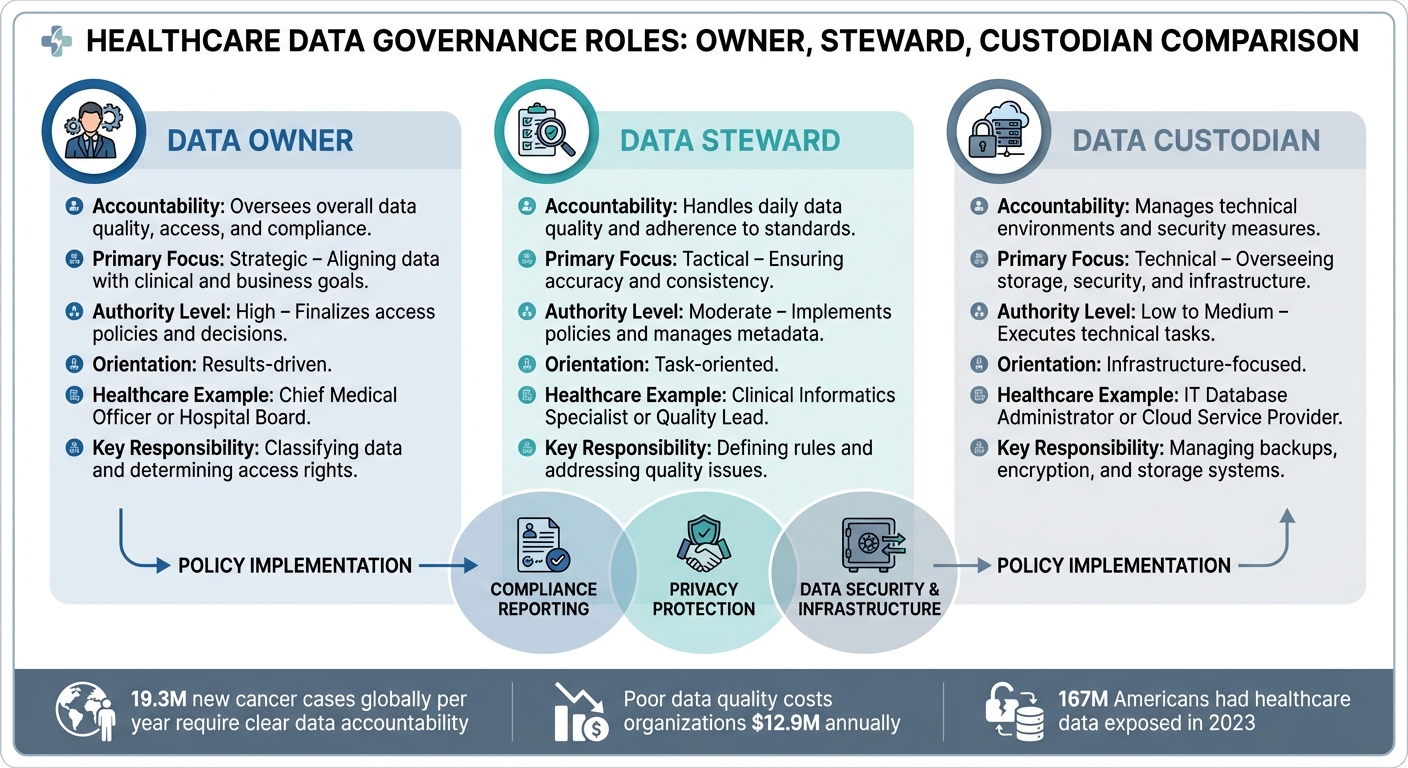
Healthcare Data Governance Roles: Owners vs Stewards vs Custodians Comparison
In data governance, clearly defined roles help manage sensitive patient information effectively. Each role operates at a different level within an organization, focusing on unique aspects of data management. This breakdown highlights their individual contributions to healthcare data governance.
Role Comparison Table
| Feature | Data Owner | Data Steward | Data Custodian |
|---|---|---|---|
| Accountability | Oversees overall data quality, access, and compliance | Handles daily data quality and adherence to standards | Manages technical environments and security measures |
| Primary Focus | Strategic – Aligning data with clinical and business goals | Tactical – Ensuring accuracy and consistency | Technical – Overseeing storage, security, and infrastructure |
| Authority Level | High – Finalizes access policies and decisions | Moderate – Implements policies and manages metadata | Low to Medium – Executes technical tasks |
| Orientation | Results-driven | Task-oriented | Infrastructure-focused |
| Healthcare Example | Chief Medical Officer or Hospital Board | Clinical Informatics Specialist or Quality Lead | IT Database Administrator or Cloud Service Provider |
| Key Responsibility | Classifying data and determining access rights | Defining rules and addressing quality issues | Managing backups, encryption, and storage systems |
The distinctions between these roles are crucial, especially given the scale of healthcare data. For instance, with 19.3 million new cancer cases reported globally each year [5], ensuring clear accountability is essential. To grasp the enormity of healthcare data, consider this: reaching one petabyte of data using standard smartphone photos (6MB each) would require taking 9,805 photos daily for 50 years [5].
Where Roles Overlap
While the table highlights their differences, these roles also intersect in critical areas. Collaboration is essential for effective data governance, particularly in compliance reporting. Here’s how they work together:
- Compliance Reporting: Data Owners ensure accountability, Stewards validate the accuracy of data, and Custodians provide audit logs.
- Policy Implementation: Owners establish policies, Stewards enforce them, and Custodians maintain the infrastructure to support these policies.
- Privacy Protection: Owners define data sensitivity, Stewards manage classification, and Custodians implement encryption and other technical safeguards.
Healthcare data governance adds another layer of complexity. Clinicians often serve as both data producers and users, while technology vendors frequently act as "stewards by design." A key area of overlap is identity resolution. For example, Data Stewards must identify when different records refer to the same patient - like prescriptions filled at multiple pharmacies - to avoid harmful drug interactions and ensure patient safety [14]. Data Custodians provide the systems to link these records, while Data Owners authorize the policies that guide patient identity matching.
This interconnected system ensures that healthcare data is managed efficiently, securely, and in compliance with regulatory standards.
How to Improve Collaboration Between Roles
Effective collaboration is the backbone of successful healthcare data governance. When data owners, stewards, and custodians work together seamlessly, healthcare organizations can avoid duplicated efforts, compliance lapses, and clinician burnout - issues that directly affect patient care and operational success. Achieving this requires a mix of clear role definitions, structured policies, and the right technology.
Setting Clear Role Boundaries
Collaboration starts with defining responsibilities through formal governance frameworks. Healthcare organizations should adopt policies that clearly outline who is Responsible, Accountable, Consulted, and Informed (RACI) for every data domain [16][17]. This prevents the common mistake of centralizing all responsibilities in one place. As Tom Varghese, Global Product Marketing & Growth Manager at Orion Health, puts it:
"Effective stewardship depends not on concentrating responsibility in one place, but on clearly articulating how these responsibilities connect and overlap" [2].
For smaller practices, governance might be informal, with a single manager juggling multiple roles. Larger organizations, however, need a formal standing committee with backing from executives. This committee should bring together representatives from billing, clinical, IT, and administrative departments, ensuring diverse perspectives are included throughout the data lifecycle [15].
Another critical step is creating a unified data glossary and metadata registry. This document standardizes every data element, specifying its format and who has the authority to modify it [15]. For instance, it should clarify whether terms like "high blood pressure" and "hypertension" refer to the same concept. Standardized terminology ensures that data owners and technical custodians are aligned [17].
Additionally, a documented communication plan is essential. Tools like email read-receipts or signed memos can confirm that staff understand their roles when policies are updated [15]. Together, these measures establish a solid foundation for collaboration.
Using Technology to Support Collaboration
Technology plays a pivotal role in streamlining data governance. Platforms designed for healthcare organizations automate workflows and create a centralized source of truth. For example, Censinet RiskOps™ supports role-based governance by enabling data owners to set access policies, stewards to oversee data quality, and custodians to enforce technical controls - all within one system. This is especially useful for managing third-party risks, where clear role definitions can prevent security breaches.
Governance platforms also provide data lineage visualization, which allows custodians to trace technical issues down to specific data columns. At the same time, data owners can track how information flows through downstream systems [16][17]. This is crucial when you consider that poor data quality costs organizations an average of $12.9 million annually and that 167 million Americans had their healthcare data exposed in cyberattacks in 2023 [17].
Another key feature is role-based access control (RBAC). This ensures that only authorized personnel can access specific data, reducing the risk of unauthorized disclosures. Such breaches led to over $4 million in fines issued by the U.S. Office for Civil Rights in 2023 alone [16][17]. By leveraging these tools, healthcare organizations can enhance collaboration while safeguarding sensitive data.
Conclusion
Healthcare data governance goes beyond meeting SOC 2 compliance requirements - it's about safeguarding patient information and enhancing the quality of care. Each role in the governance framework plays a critical part. Data owners establish policies and bear ultimate accountability. Data stewards focus on maintaining the accuracy and usability of data on a daily basis, while data custodians handle the technical infrastructure and enforce security protocols.
When these roles work in harmony, the results are tangible. Organizations can avoid errors linked to over 250,000 deaths annually in the U.S. and prevent breaches like the one at New York-Presbyterian Hospital in 2014, which exposed 6,800 patient records and resulted in a $4.8 million penalty due to insufficient safeguards [18].
This approach also highlights the ethical responsibility of data governance. As Tom Varghese from Orion Health puts it:
"When stewardship is narrowly defined as compliance or efficiency, systems fracture, and people suffer. When it is understood as a collective ethical responsibility, health data becomes a shared asset" [2].
Policies provide the structure, and technology brings them to life. Platforms like Censinet RiskOps™ allow data owners to define access, data stewards to maintain data quality, and data custodians to secure systems - all within a unified framework. This alignment is crucial, especially given that nearly 33% of the world’s data is generated by the healthcare industry [10].
FAQs
Who is ultimately accountable when healthcare data is misused or breached?
The person designated as the data owner carries the ultimate responsibility for any misuse or breaches of healthcare data. Typically, this role is assigned to senior management or a department head. They are tasked with establishing controls and ensuring that sensitive information is handled appropriately and securely.
How do we decide which datasets need a Data Owner, Steward, and Custodian?
Deciding which datasets need a Data Owner, Steward, and Custodian comes down to factors such as data sensitivity, regulatory requirements, and the organization's goals.
- Data Owners are responsible for overseeing the data's quality, ensuring proper access controls, and maintaining compliance with policies and regulations.
- Data Stewards focus on the daily management of data quality and making sure policies are applied consistently.
- Custodians take care of the technical side, including data storage, security, and system maintenance.
Assigning these roles is key for maintaining accountability and strong governance, particularly for datasets that are critical or sensitive.
What’s the best way to prevent role confusion between IT and clinical teams?
To prevent role confusion between IT and clinical teams, it's crucial to define clear responsibilities for data owners, stewards, and custodians. This can be achieved by implementing detailed data governance policies that outline everyone's duties. Encouraging open communication and teamwork helps clarify any overlaps and establish boundaries. Additionally, training programs and risk management tools can reinforce these roles, improve workflow efficiency, and ensure everyone stays aligned with organizational policies and compliance requirements.


